Caps come with instructions. They may have video instructions which can be easier to follow than written instructions. Check the product information leaflet for a link to video instructions.
This guide can help you put in a FemCap, which is the only brand of cap currently available in the UK. The different sizes of FemCap are all used in the same way.
It’s advised that you also get advice from a healthcare professional before using a cap – also see above – How do I learn to use my diaphragm or cap?
Wash your hands before putting in a cap.
The cap needs to cover your cervix. It’s helpful to feel your cervix before inserting the cap – see above – How do I find my cervix?
You might squat, lie down, or stand with one foot up on a chair while putting your cap in, like you would when putting in a tampon or menstrual cup. Choose the position that’s easiest for you.
- Hold the cap with the strap underneath and the narrower part of the cap at the top.
- Fill about one-third of the cap with contraceptive gel or spermicide. This is the part that will go against your cervix. Don’t put any contraceptive gel or spermicide around the rim (outer edge) as this may stop the cap staying in place.
- The side of the cap with the strap has space between the dome and the rim. Put some contraceptive gel or spermicide in this space.
- Squeeze the sides of the cap together and hold the cap between your thumb and first 2 fingers.
- Hold the cap with the strap underneath and the wider side of the cap pointing downwards and towards your back.
- Still squeezing it together, slide the cap into your vagina upwards and backwards as far as it will go.
- It needs to completely cover the cervix.
- It’s held in place by suction and supported by the sides of the vagina.
- Use a finger to feel for your cervix. If you can feel it, then it isn’t covered. Take the cap out by hooking your finger under the strap and gently pulling downwards. Then try again.
Always add more contraceptive gel or spermicide before having sex if the cap has been in place for more than 2 hours. Keep the cap in your vagina and use your finger or an applicator to add more gel or spermicide.
Leave the cap in for at least 6 hours after sex. If you want to have sex again during this time, always add more contraceptive gel or spermicide first. Keep the cap in your vagina and use your finger or an applicator to add more gel or spermicide.



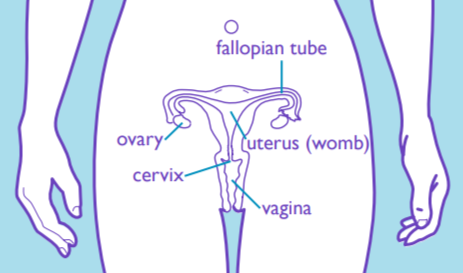 A diaphragm or cap is put into the top of your vagina. It covers your cervix, which is the entrance to the uterus (womb).
A diaphragm or cap is put into the top of your vagina. It covers your cervix, which is the entrance to the uterus (womb).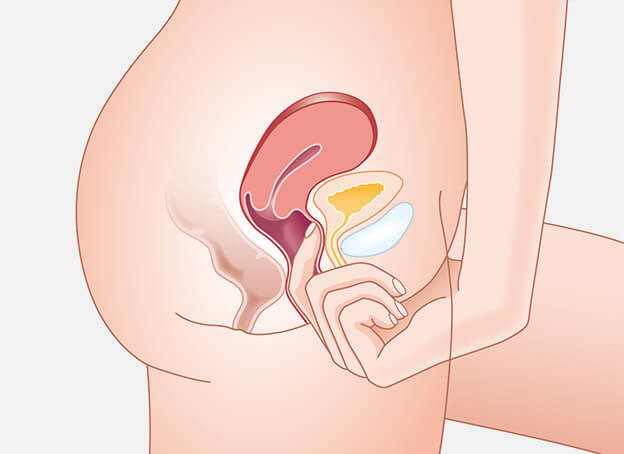 You can find your cervix by inserting a clean finger into your vagina until you touch the top and can’t go any further. The cervix feels like the end of your nose.
You can find your cervix by inserting a clean finger into your vagina until you touch the top and can’t go any further. The cervix feels like the end of your nose.


 Leave in your diaphragm or cap for at least 6 hours after the last time you had sex.
Leave in your diaphragm or cap for at least 6 hours after the last time you had sex.
