Discovering the Gufasha Girl Foundation
It astounds us here at FPA how some people find the time to help so many positive causes and help so many people.
Below – an update from Dr Becky Foljambe – GP, FPA Ambassador, founder of the You Before Two charity and so much more – on how she’s been supporting the Gufasha Girl Foundation in Uganda.
Before we begin, we’d like to warn you that this piece contains references to child marriage and pregnancy, abortion, and extreme poverty which some readers may find upsetting.
“My time with Joan Kembabazi was time well spent.”
It is incredible moments like those I spent in Uganda in June of this year with the inspirational Joan Kembabazi, founder of the Gufasha Girl Foundation (GGF), that will root my feet to the ground for decades to come. Some trips in life just change us. This was one of those trips.
Connecting with Joan Kembabazi
I had first come across Joan in a webinar where we were both asked to participate in, ‘Is education the magic bullet?’ hosted by the charity Population Matters.
I was Vice Chair for the board at the time but had been asked to speak based on my own work and life experience of the issues facing women and girls of reproductive age today.
That day I was imparting some grim statistics from the UK on screen to Joan in Uganda and the other speakers in Austria and Nigeria.
45% of pregnancies in Britain are unplanned or ambivalent
‘Teenage conception rates in England and Wales have been continuing to rise since 2021-reversing the previous fourteen years of improvement.’ (Dr Janet Barter, the FSRH President’s open letter to Wes Streeting, Secretary of State for Health and Social Care).
In fact, 45% of all pregnancies in Britain are unplanned or ambivalent. Among other things, I talked about the plateau in teenage pregnancies (which as I write now are on the way back up), along with teenage abortion rates.
In Uganda child marriage and teenage pregnancy go hand-in-hand
Then to Joan! She told us about Uganda ranking as the 31st most densely populated country in the world. 34% of girls are married before the age of 18 and 64% of girls have engaged in sexual activity before the age of 18.
‘Child marriage and teenage pregnancy go hand-in-hand’ Joan told us.
It’s the inevitability of giving birth once married that was a worrying message here. Futures for these very young women are instantly defined and, after getting married, they often ‘give birth almost immediately’.
‘An educated girl will get married later and have children later in life’ Joan said. We know this is a universal theme.
The issues Joan and her GGF team face are pronounced. She relayed the findings from a rapid assessment survey in February 2023: 2 in 5 girls (age 13-16) were pregnant and 1 in 5 girls had already given birth at the time. These girls were from the communities that Joan works with in the Kayunga district.
‘The lack of education is really making girls get married at a very young age.’
Listening to Joan it was clear that ending child marriage and child pregnancy is such an important part of stabilising fertility rates in Uganda and allowing girls to thrive and pursue their own lives.
Joan talked about the fact ‘we need to go beyond the classroom,’ and the need to ‘help girls make choices for their own lives, for their own bodies.’ Advocating for this extends to advocating for climate justice and gender equality.
I knew that hearing Joan for the first time that day, only in her early twenties, that she had a deep wisdom, knowledge and empathy for her fellow girls in Uganda and around the world. I also knew we had to meet!
So, when I got the chance to visit her in her home district of Kayunga in June this year, I leapt at it!
Visiting Uganda
The warmest of arrivals at Entebbe airport greeted me and my husband Ralph – women are advised not to travel alone in Uganda.
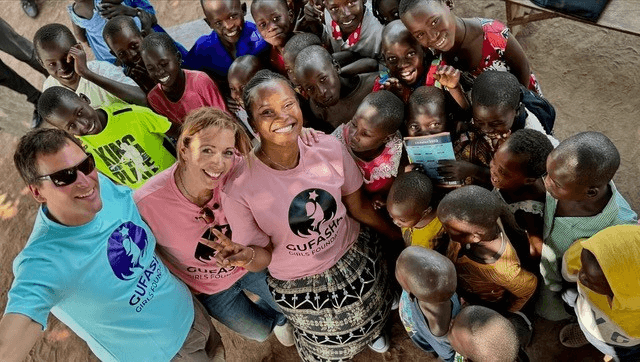
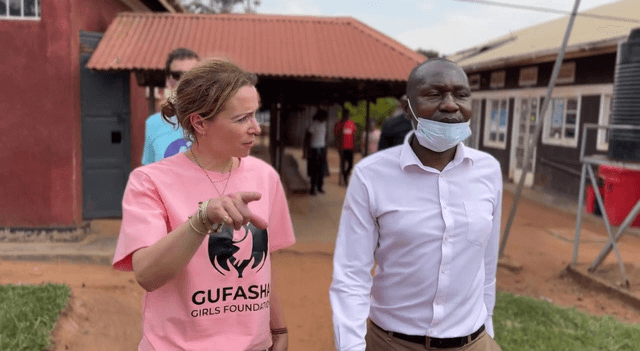
Joan and her superstar GGF team member Jamil, who we would get to know well over the next few days, threw a Ugandan flag over our shoulders and I got to give Joan a hug for the first time.
The reception we received in all the places Joan and Jamil took us to was warmer than we felt we’d ever had anywhere! Happy hours were spent driving down dusty roads out of Kampala to Kayunga, the district where Joan grew up and still lives.
We visited Joan and her community in the village of Namirembe, a small but buzzing community, entirely self-built with a water pump to supply the village, electricity only through small solar panels on thatched roofs, enough to light a single bulb, and food a scarcity hard earned and carefully shared.
There were many children running around with huge smiles and excited chatter, that defied the difficulties this community faces every day.
They were inspiring beyond measure and clearly immensely proud of what Joan has achieved since the death of her best friend Moureen Gufasha, who died in childbirth at age 13.
Moureen Gufasha is the namesake of the Foundation.
The grief that must have hit Joan and her community so hard has powered Joan to create change.

Helping women and girls with educational and economic empowerment
We were introduced to some of the women and girls she has since helped through educational and economic empowerment programmes and school sponsorship.
We visited some of the local schools and the girls Joan is supporting to fulfil a proper education:
- Bbaale Subcounty, Divine Embassy Primary School where we met Angel, who wishes to become a doctor
- Pride Junior School where we met Margaret and Grace, all doing well in their studies thanks to GGF sponsorship

Then to Bbaale Health Centre IV (the hospital), where we were greeted by Dr Noah, the doctor in charge. Speaking to the tireless clinical staff there deeply shocked me. It took me some time to fully realise why. As one would sadly expect, the resources were poor in comparison to the ‘health wealth’ of the UK.
As a doctor used to working in clinics that might not be desirably cool, calm and clean by our standards, but are essentially adequate to all extents and purposes. These rooms were the opposite.
Despite the evident buzz of clinical activity tending to patients in a caring way, there was no possibility of segregating patients.
Feverish children and babies were on a ward with adult patients suffering with psychosis, malaria, or chest and urine infections.
Beds were being shared and staff to patient ratios were inappropriate, but that did not stop any patients I saw calmly and politely waiting for care, given by diligent and attentive staff.
I visited the maternity building where heavily pregnant women of all ages sat for hours patiently waiting on stone benches in the heat.
A tirelessly jolly midwife ushered each patient into her tiny, cluttered room with a skilled and unflappable calmness despite all the obvious challenges they must face each day.
The patients themselves had travelled often by foot for miles and many hot hours, no transport, no support, no smartphones!
Contraceptive Implants and HIV Tests
I was shown the room where cervical smears were regularly taking place, and I was delighted to see a pop-up tent offering on-site HIV tests.
There were no computerised records for the contraception given, just a huge logbook. I was allowed to turn the pages and see a log of all the female patients, with the dates and types of contraception they had been given.
Contraceptive implants being the most popular and depo progesterone contraceptive injections, which can be self-administered (sayana press).
In Uganda the hormonal IUD (coil) insertions were infrequent due to the practical implications of inserting them and the risk of infection Dr Noah told me.
As I flicked through the pages and saw hundreds of entries in the book, a mother sat to my left cradling a 4-day old baby following an emergency section whilst the nurse injected her arm with a hefty syringe full of antibiotics.
Thinking about the Western World
It was at this moment when I realised what ‘meeting patient needs’ is in its purest form. What we try to do in the UK now is too elaborate and has moved too far from a position of gratitude. This runs very deep in my view.
The politicians have become so aspirational in their views of sexual health services whilst at the same time stripping its funding.
Then to the later thoughts that I needed time to fully grapple with.
The intolerance and ingratitude of us in the Western World, and yes that includes the UK, where we have contraception free at the point of access and clinics (albeit scantier in numbers) that are within a couple of hours’ drive at most, offering a full range of free sexual health care.
I would argue that we and the omnipresent online world (Kayunga children do not have smartphones, they don’t even have toothbrushes), are teaching our young women to be intolerant of symptoms associated with healthy periods and menopause. We have raised expectations of contraception and any side effects.
There have also been appalling viral moments of misinformation over the past ten years, not least this astonishingly irresponsible tweet from Elon Musk earlier this year viewed 43.9 million times with 192,500 likes.
It is little wonder when faced with such unfounded and irresponsible public messaging that we are now seeing on a daily basis at work young women who want to:
- ‘rest their bodies from contraception’ (myth)
- ‘stop contraception as they’re worried it has decreased their fertility’ (another myth)

Or softer but no less influential issues for girls that makes them stop or change their contraception, e.g. it makes them feel a ‘bit bloated,’ ‘a bit moody,’ or ‘bleed a bit and it’s annoying.’
Please don’t get me wrong I am not encouraging anyone to take contraception that doesn’t suit them or makes them feel unwell.
However, I think as contraception takers and issuers in the UK we have stopped asking ourselves ‘do I want an unplanned pregnancy?’ and are now focussing more on ‘how do I feel on my contraception?’
This latter question simply is not asked to the same extent in places like Bbaale hospital, because these women know that without contraception their lives will be immeasurably worse.
They cannot afford such luxurious contemplation, and because of this (and many other reasons) they have so much to teach us here in the UK.
Dr Becky’s Takeaway…
There is a refreshing, frank and pragmatic attitude to reproductive health in Uganda.
We are all talking about reproductive rights, that is clear, but when looking at what’s truly at stake in places like Kayunga when these rights are abused, we should not be shying away from conversations that prioritise contraception and access to abortion.
As women we must walk in other women’s shoes across the world. I was so privileged to be able to do this with Joan. Her work is quite literally saving girls’ lives through education, the most powerful tool in the fight for their safety, rights and autonomy.
We save the girls, and we save society

Supporting girls and women: Gufasha Girl Foundation
According to Joan, ‘Girls and women have a right to access the tools and resources they need to choose for their bodies and their lives.’
At the FPA we couldn’t agree more. But the work is far from over.
If you’d like to support the Gufasha Girl Foundation you make a direct donation here: https://gufashagirls.org/donate/
Thank you





